SKIN ALLERGY/UTICARIA /कर्कश, पित्ती
 Ewing Sarcoma | 24/05/2022
Ewing Sarcoma | 24/05/2022

What is urticaria?
Urticaria is characterised by very itchy weals (hives), with or without surrounding erythematous flares. The name urticaria is derived from the common European stinging nettle Urtica dioica. Urticaria can be acute or chronic, spontaneous or inducible.
A weal (or wheal) is a superficial skin-coloured or pale skin swelling, usually surrounded by erythema that lasts anything from a few minutes to 24 hours.
Urticaria can co-exist with angioedema which is a deeper swelling within the skin or mucous membranes.
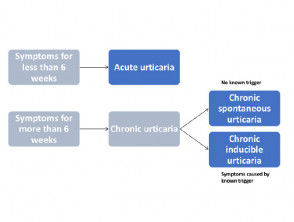
Classification of urticaria
Urticaria is classified according to its duration.
- Acute urticaria (< 6 weeks duration, and often gone within hours to days)
- Chronic urticaria (> 6 weeks duration, with daily or episodic weals)
Chronic urticaria may be spontaneous or inducible. Both types may co-exist.
Classification of urticaria
Chronic inducible urticaria includes:
- Dermographism
- Cold urticaria
- Cholinergic urticaria
- Contact urticaria
- Delayed pressure urticaria
- Solar urticaria
- Heat urticaria
- Vibratory urticaria
- Vibratory angioedema
- Aquagenic urticaria
Who gets urticaria and why?
One in five children or adults has an episode of acute urticaria during their lifetime. It affects all races and both sexes.
Acute urticaria can occur in newborns and infants but is uncommon. Acute urticaria in children is usually caused by infection, even if afebrile. In older children food, medication, and inhaled allergens are also important causes. In adults urticaria is usually idiopathic and spontaneous.
Acute urticaria with fever can be the first sign of COVID-19 infection.
Chronic spontaneous urticaria affects 0.5–2% of the population; in some series, two-thirds are women. Chronic inducible urticaria is however more common. There are genetic and autoimmune associations.
What are the clinical features of urticaria?
Urticarial weals can be a few millimetres or several centimetres in diameter, coloured white or red, with or without a red flare. Each weal may last a few minutes or several hours and may change shape. Weals may be round, or form rings, a map-like pattern, or giant patches.
Urticaria can affect any site of the body and tends to be distributed widely.
Angioedema is more often localised. It commonly affects the face (especially eyelids and perioral sites), hands, feet, and genitalia. It may involve tongue, uvula, soft palate, or larynx.
Serum sickness due to blood transfusion and serum sickness-like reactions due to certain drugs cause acute urticaria leaving bruises, fever, swollen lymph glands, joint pain and swelling.
In chronic inducible urticaria, weals appear about 5 minutes after the stimulus and last a few minutes or up to one hour. Characteristically, weals are:
- Linear in dermographism
- Tiny in cholinergic urticaria
- Confined to contact areas in contact urticaria
- Diffuse in cold urticaria—if large areas of skin are affected, they can lead to fainting (potentially dangerous if swimming in cold water).
The weals are more persistent in chronic spontaneous urticaria, but each individual lesion will resolve within 24 hours. They may occur at certain times of the day.
What causes urticaria?
Weals are due to release of chemical mediators from tissue mast cells and circulating basophils. These chemical mediators include histamine, platelet-activating factor and cytokines. The mediators activate sensory nerves and cause dilation of blood vessels and leakage of fluid into surrounding tissues. Bradykinin release causes angioedema.
Several hypotheses have been proposed to explain urticaria. The immune, arachidonic acid and coagulation systems are involved, and genetic mutations are under investigation.
Acute urticaria
Acute urticaria can be induced by the following factors, but the cause is not always identified.
- Acute viral infection — upper respiratory infection, viral hepatitis, infectious mononucleosis, mycoplasma
- Acute bacterial infection — dental abscess, sinusitis
- Food allergy (IgE mediated)—usually milk, egg, peanut, shellfish
- Drug allergy (IgE mediated drug-induced urticaria) — often an antibiotic
- Drug-induced urticaria due to pseudoallergy — aspirin, nonselective nonsteroidal anti-inflammatory drugs, opiates, radiocontrast media; these cause urticaria without immune activation
- Vaccination
- Bee or wasp stings
- Widespread reaction following localised contact urticaria — for example, latex
Severe allergic urticaria may lead to anaphylactic shock (bronchospasm, collapse).
Immune complexes due to blood transfusion cause serum sickness and certain drugs cause serum sickness-like reactions.
A single episode or recurrent episodes of angioedema without urticaria can be due to an angiotensin-converting enzyme (ACE) inhibitor drug [see ACE inhibitor-induced angioedema].
Chronic urticaria
Chronic spontaneous urticaria is mainly idiopathic (cause unknown). An autoimmune cause is likely. About half of investigated patients carry functional IgG autoantibodies to immunoglobulin IgE or high-affinity receptor FcεRIα.
Chronic spontaneous urticaria has also been associated with:
- Chronic underlying infection, such as Helicobacter pylori (bowel parasites)
- Chronic autoimmune diseases, such as systemic lupus erythematosus, thyroid disease, coeliac disease, vitiligo, and others.
Weals in chronic spontaneous urticaria may be aggravated by:
- Heat
- Viral infection
- Tight clothing
- Drug pseudoallergy—aspirin, nonsteroidal anti-inflammatory drugs, opiates
- Food pseudoallergy—salicylates, azo dye food colouring agents such as tartrazine (102), benzoate preservatives (210-220), and other food additives.
Inducible urticaria is a response to a physical stimulus.
How is urticaria diagnosed?
Urticaria is diagnosed in people with a history of weals that last less than 24 hours with or without angioedema. A medication and family history should be elicited. A thorough physical examination should be undertaken.
Skin prick tests and radioallergosorbent tests (RAST) or CAP fluoroimmunoassay may be requested if a drug, latex, or food allergy is suspected in acute urticaria.
There are no routine diagnostic tests in chronic spontaneous urticaria apart from blood count and C-reactive protein (CBC, CRP), but investigations may be undertaken if an underlying disorder is suspected.
The autologous serum skin test is sometimes carried out in chronic spontaneous urticaria, but its value is uncertain. It is positive if an injection of the patient's serum under the skin causes a red weal.
Inducible urticaria is often confirmed by inducing the reaction eg, scratching the skin in dermographism or applying an ice cube in suspected cold urticaria.
Investigations for a systemic condition or autoinflammatory disease should be undertaken in urticaria patients with fever, joint or bone pain, and malaise. Patients with angioedema without weals should be asked if they take ACE inhibitor drugs and tested for complement C4; C1-INH levels, function and antibodies; and C1q.
Biopsy of urticaria can be non-specific. The pathology shows oedema in the dermis and dilated blood vessels, with a variable mixed inflammatory infiltrate. Vessel-wall damage indicates urticarial vasculitis.
What is the treatment for urticaria?
The main treatment of all forms of urticaria in adults and children is with an oral second-generation H1-antihistamine such as cetirizine or loratidine. If the standard dose (eg, 10 mg for cetirizine) is not effective, the dose can be increased up to fourfold (eg, 40 mg cetirizine daily). They are stopped when the acute urticaria has settled down. The addition of a second antihistamine is not thought to be helpful.
Terfenadine and astemizole should not be used, as they are cardiotoxic in combination with ketoconazole or erythromycin. They are no longer available in New Zealand.
Although systemic treatment is best avoided during pregnancy and breastfeeding, there have been no reports that second-generation antihistamines cause birth defects. If treatment is required, loratadine and cetirizine are currently preferred.
Conventional first-generation antihistamines such as promethazine or chlorpheniramine are no longer recommended for urticaria.
Avoidance of trigger factors
Identified triggers should be eliminated if possible (eg, drug or food allergy). Avoidance of relevant type 1 (IgE-mediated) allergens clears urticaria within 48 hours.
- Treat identified chronic infections such as H. pylori.
- Avoid aspirin, opiates and nonsteroidal anti-inflammatory drugs (paracetamol is generally safe).
- Minimise dietary pseudoallergens for a trial period of at least three weeks.
- Avoid known allergens that have been confirmed by positive specific IgE/skin prick tests if these have clinical relevance for urticaria.
- Cool the affected area with a fan, cold flannel, ice pack, or soothing moisturising lotion.
The physical triggers for inducible urticaria should be minimised; see examples below. However, symptoms often persist.
- Symptomatic dermographism: reduce friction eg, avoid tight clothing.
- Cold urticaria: dress warmly in cold or windy conditions and avoid swimming in cold water.
- Delayed pressure urticaria: broaden the contact area eg, of a heavy bag.
- Solar urticaria: dress up and apply broad-spectrum sunscreens.
Some patients with inducible urticaria benefit from daily induction of symptoms to induce tolerance. Phototherapy may relieve the itch of symptomatic dermographism.
Treatment of acute refractory urticaria
If non-sedating antihistamines are not effective, a 4 to 5-day course of oral prednisone (prednisolone) may be warranted in severe acute urticaria.
Intramuscular injection of adrenaline (epinephrine) is reserved for life-threatening anaphylaxis or swelling of the throat.
Treatment of chronic refractory urticaria
Patients with chronic urticaria that has failed to respond to maximum-dose second-generation oral antihistamines taken for four weeks should be referred to a dermatologist, immunologist or medical allergy specialist.
There is good evidence to support treatment with omalizumab or ciclosporin, which each have a 65% response rate in antihistamine-resistant patients.
Long-term systemic corticosteroids are not recommended, as high doses are required to reduce symptoms of urticaria and they have inevitable adverse effects that can be serious.
The effectiveness of treatment can be objectively monitored using urticaria control test. Patients are asked to score the physical symptoms of urticaria they have experienced in the previous four weeks, quality of life affected by urticaria, how often treatment was not enough to control symptoms, and overall control of urticaria.
What is the differential diagnosis of urticaria?
- Scombroid fish poisoning
- Papular urticaria
- Mastocytosis
- Urticarial vasculitis
- Autoinflammatory syndromes
What is the outlook for chronic urticaria?
Acute urticaria resolves in hours to days but is often recurrent. Although chronic urticaria clears up in most cases, 15% continue to have wealing at least twice weekly after two years.
Bibliography
- Cicardi M, Aberer W, Banerji A, et al. Classification, diagnosis, and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy. 2014;69(5):602–16. doi:10.1111/all.12380. PubMed
- Grattan CE, Humphreys F; British Association of Dermatologists Therapy Guidelines and Audit Subcommittee. Guidelines for evaluation and management of urticaria in adults and children. Br J Dermatol. 2007;157(6):1116–23. doi:10.1111/j.1365-2133.2007.08283.x PubMed
- Greenberger PA. Chronic urticaria: new management options. World Allergy Organ J. 2014;7(1):31. doi:10.1186/1939-4551-7-31. Journal
- Jáuregui I, Ortiz de Frutos FJ, Ferrer M, et al. Assessment of severity and quality of life in chronic urticaria. J Investig Allergol Clin Immunol. 2014;24(2):80–6. PubMed Central
- Maurer M, Rosén K, Hsieh HJ, et al. Omalizumab for the treatment of chronic idiopathic or spontaneous urticaria [published correction appears in N Engl J Med. 2013 Jun 13;368(24):2340–1]. N Engl J Med. 2013;368(10):924–35. doi:10.1056/NEJMoa1215372. PubMed
- Radonjic-Hoesli S, Hofmeier KS, Micaletto S, Schmid-Grendelmeier P, Bircher A, Simon D. Urticaria and angioedema: an update on classification and pathogenesis. Clin Rev Allergy Immunol. 2018;54(1):88–101. doi:10.1007/s12016-017-8628-1. PubMed
- Techasatian L, Phungoen P, Chaiyarit J, Uppala R. Etiological and predictive factors of pediatric urticaria in an emergency context. BMC Pediatr. 2021;21(1):92. doi:10.1186/s12887-021-02553-y Journal
Full article Reference :
https://dermnetnz.org/topics/urticaria-an-overview
You may also like
६३ दिन, ८ जना, ३ जिल्ला, १ प्रदेश(कर्णाली)
Doctor Story Nepal | 22/05/2022
SKIN ALLERGY/UTICARIA /कर्कश, पित्ती
Ewing Sarcoma | 24/05/2022